Acute Coronary Syndrome
Introduction
c.
Platelet glycoprotein IIb/IIIa
receptor antagonist
Acute
Coronary Syndrome (ACS) describes any constellation of clinical symptoms due to
myocardiac
ischemia. It includes acute myocardiac infarction(MI) [ST
elevation MI (STEMI)
and non-ST elevation MI (NSTEMI)
and unstable
angina.
High
risk of group :
i.New
onset (<2months)
angina that is severe
and frequent
(>3 episodes/day).
ii. Accelerating
angina ,i.e.previosly
chronic stable angina which becomes distinctly more frequent,severe, prolonges, or
precipitated by lessexertion than
before.
iii. Angina
at rest (
>20minutes)
A.
Clinical Features
&
Diagnosis
1.
Symptoms
•Chest pain/discomfort, usually
retrosternal, central or in the left chest, may radiate to jaw or down upper
limb
• May be crushing , pressing or burning
• Severity of pain is variable
• May be difficult to differentiate btw
symptoms of STEMI and UA/NSTEMI
•Left ventricular failure(some)
•Unexplain fatigue, SOB, epigastric
discomfort, nausea and vomit.
2.
Physical Examination
•To identify precipitating factors and
consequences of UA/NSTEMI
3.
Investigation
•ECG :
i.ST
segment depression >0.05 mV
ii. T
wave inversion –marked >0.2mV symmetrical T-wave inversion in pericordial
leads.
• Troponin, cardiac enzymes (CKMB, AST,
LDH)
• Echocardiography
•CXR, FBC, PT, PTT, LFT, creatinine,
BUSE, glucose, and lipid profile.
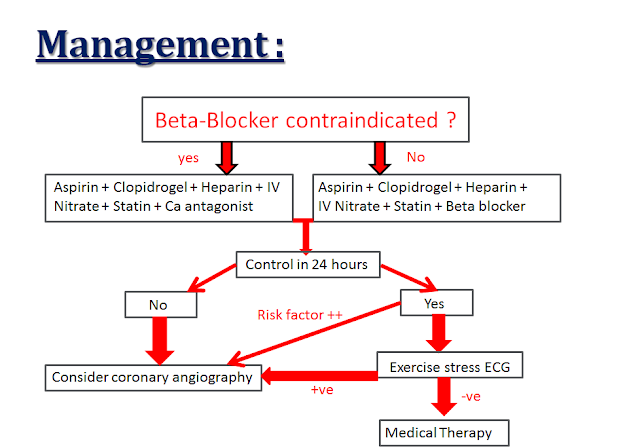
B. MANAGEMENT
1.
General Measures
•Admit to CCU for observation. Monitor
cardiac rhythm for 24-48 hr. Pt encourage to report any recurrence of
pain.
•Bed rest, sedation and analgesics should
be administered as in AMI. IV morphine is recommended for pt with
persistent or recurrrent
symptoms despite anti-ischaemic
therapy. IV morphine is given as bolus 2-5mg with IV anti-emetic e.g. IV
metoclopramide (Maxalon)
10mg. Repeat dose may be given.
•BP every 15-30 min for a few hr,then
every 1-2hr.
•IV line for drug administered.
•O2 via nasal prongs.
•Serial ECG and cardiac enzyme to detect
AMI and silent and recurrent ischemid.
•Other coronary risk factor (eg. DM,
hypercholesterolaemia)
& precipitating factor (eg,anaemia) should be treated.
2.
Anti-Thrombotic Therapy
• Combination of aspirin
(ASA), Clopidogel, unfractional
heparin (UFH)
or low
molecular weight heparin (LMWH), with or without a platelet GP IIb/IIIa
receptor antagonist is the optimal therapy.
|
Low Risk UA/ NSTE MI pt
|
High Risk UA/NSTEMI pt
|
|
ASA +
Clopidogel +
SC LMWH or
IV UFH
|
ASA +
Clopidogel +
SC LMWH or
IV UFH +
IV platelet GP IIb/IIIa antagonist
|
a. Antiplatelet agents
:
•Choice of agents:
-Cyclo-oxygenase
inhibitors : Aspirin.
-Adenosine diphosphate(ADP) receptor antagonists : Clipidogrel , Ticlopidine
•Dose :
-Aspirin 300mg chewed or crushed and swallowed for
rapid effect, then 75-150mg daily (if no contra-indication)
-Clopidrogel
300mg start followed by 75mg daily
- Ticlopidine 250mg (for aspirin hypersensitivity and
intolerance). Associated with neutropenia in 2% of pt. Monitoring of FBC (2-4
weekly for the first 3-4months) is important.
b.
Anticoagulants
•IV
unfractionated Heparin (UFH) decreases incidence of MI in pt with
UA. It
is given as bolus dose of 5000 U followed by infusion of 1000
U per
hour. The infusion rate is adjusted by regular monitoring of aPTT,
keeping it to 1.5-2.5X control.
This should be maintained for 2-5 days.
•Low molecular weight heparin (LMWH)
available include dalteparin, nadroparin
( Fraxiparine)
& enoxaparin
( Clexane).
|
Recommended
Dosage
|
||
|
UFH
|
IV
Bolus
|
•80 U/kg (maximum of 5000 U)
•Infusion of 18U/kg/h (max 1000)
|
|
Target
aPTT
|
•1.5-2.5
times or approximately 60-80s
•It
should be monitored and measured
|
|
|
LMWH
|
Enoxaprin ( Clexane)
Nadroparin ( Fraxiparine)
|
•1mg/kg 5C.bd*
•0.1 ml/ 10kg.5C.bd*
|
|
RECOMMENDED DOSAGE
|
The dosing regime for the initial
phase pharmacological
therapy preceeding PCl(upstream use) & during PCl
are as follow:
|
|
|
1.Abciximab
(Reopro)
|
Upstream use & planned
PCI
PCI
|
•IV
Bolus 0.25mg/kg h before procedure.
•Follow by continuous infusion of 0.125µg/kg
per min (to a max of 10µg/min) for 12 h.
•
•IV
Bolus 0.25mg/kg h for 10-60min before the start of PCI
•Followed by continuous infusion
of 0.125µg/kg per min(to a maxi of 10µg/min) for 12 h.
|
|
2. Eptifibatide (Integrilin)
|
PCI
|
•IV
Bolus 180µg/kg
•Immediately followed by a
2µg/kg/min infusion
•Then a second 180µg/kg bolus
10min later.
•The infusion should be continued
until hospital discharge ,up to 18-24h.
•
|
|
|
||
|
2. Eptifibitide
|
Upstream use
|
•IV Bolus 180µg/kg (max 22.6mg) over
1-2min
•Follow by
an infusion of 2µg/kg /min ( max of 15mg/h) for 72h or until hospital
discharge .
•In the cases of PCI, the infusion
should be continued for 96h.
|
|
3. Tirofiban
(Aggrastat)
|
Upstream use
PCI
|
•IV
Bolus 0.4µg/kg /min for 30min
•Follow by an infusion of 0.1 µg/kg /min for
48-108h
•In the cases of PCI, the infusion
should be continued 12-24h after PCI.
•
•IV
Bolus of 25µg/kg given over 3-7min (max 10ml/min)
•Follow by maintenance infusion of 0.15µg/kg
/min for 8-10h post PTCA
|
Comments
Post a Comment