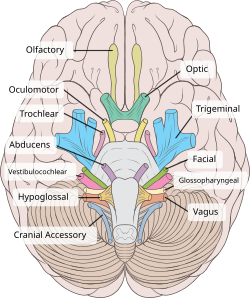
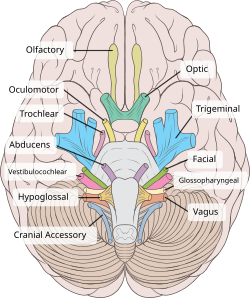
cranial nerve
12 cranial nerve
mneumonics to remember it..
Oh Oh Oh, To Touch And Feel Very Green Vagina Ah Ha!!
I . Olfactory Nerve
 foramina on the cribriform plate
foramina on the cribriform plate
Testing Technique
Olfactory Defect:
Hyperosmia is increased olfactory acuity, and
hypoosmia is diminished olfactory acuity.
Anosmia, the inability to recognize odors, may be unilateral or bilateral.
Dysosmia is an abnormal sense of smell.
II. Optic Nerve
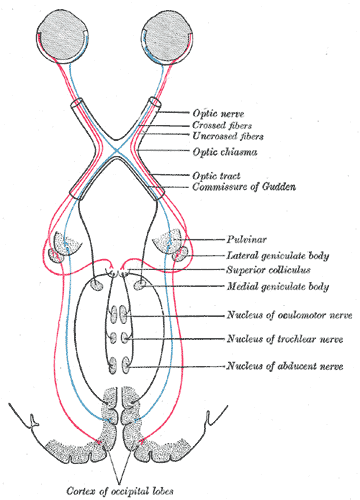

Transmits visual information from the retina to the brain. Derived from the embryonic retinal ganglion cell.
what is retinal ganglion cell.?
as we learn from histology...
It located in ganglion cell layer...whereby it consist few types of ganglion cell..lets c few types of it..(from wiki)

III. Oculomotor Nerve
enter via superior orbital fissure and controls most of the eye's movements, including constriction of the pupil and maintaining an open eyelid
nnervates a single muscle: the superior oblique muscle..
Nucleus:
control lateral rectus mucle of the eye.
enter through superior orbital fissure.
 abducens nucleus is located in the pons, on the floor of thefourth ventricle, at the level of the facial colliculus
abducens nucleus is located in the pons, on the floor of thefourth ventricle, at the level of the facial colliculus
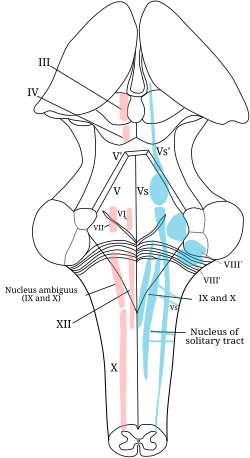
V. Trigeminal Nerve
first of all,There is 3 branches for trigeminal nerve.
V1.Opthalmic
V2. maxillary
V3 Mandibular.



 3
3


VII. Facial Nerve

Most important 5 branches.. temporal,zygomatic,buccal,mandibular,cervical...

Branches:(from wiki)
Temporal branches of the facial nerve, a patient is asked to frown and wrinkle his or her forehead.
Zygomatic branches of the facial nerve, a patient is asked to close their eyes tightly.
VIII. Vestibulocochlear Nerve
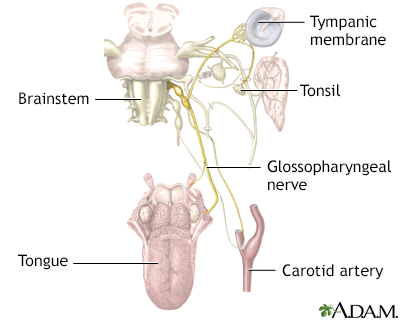
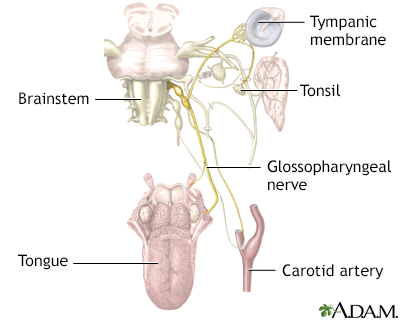
IX. Glossopharyngeal Nerve

 \
\


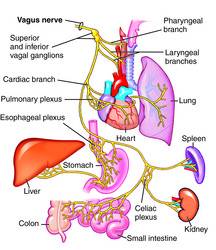
X. Vagus Nerve
XI. Spinal Accessory
XII. Hypoglossal Nerve
mneumonics to remember it..
Oh Oh Oh, To Touch And Feel Very Green Vagina Ah Ha!!
I . Olfactory Nerve
 foramina on the cribriform plate
foramina on the cribriform plate
Testing Technique
Carry a vial of a nonirritating substance in your bag; vanilla, lemon, and freshly ground coffee are good examples, and tobacco or scented soap will do if necessary. These odors stimulate the olfactory receptors. Do not use irritating odors such as camphor or menthol. These substances stimulate the trigeminal sensory receptors in addition to the olfactory receptors, potentially giving a false result.
Inform the patient that you are going to test the sense of smell. The patient places an index finger over one nostril to block it (e.g., right index finger over right nostril). He or she then closes the eyes. Instruct the patient to sniff repetitively and to tell you when an odor is detected, identifying the odor if recognized. Bring the test odor up to within 30 cm or less of the nose. Do not touch the patient when doing the test. Movement of your body will give a clue as to when the test object is being presented. Do not give auditory clues. Repeat the process with the other nostril. Smell is intact when the patient reports detection of an odor. Recognition of the odor involves olfactory memory, which is a higher cortical function.
Olfactory Defect:
Hyperosmia is increased olfactory acuity, and
hypoosmia is diminished olfactory acuity.
Anosmia, the inability to recognize odors, may be unilateral or bilateral.
Dysosmia is an abnormal sense of smell.
Table 59.1Examples of Disorders Reported To Be Associated with Olfactory Dysfunction
| Endocrine |
| Adrenal cortical insufficiency |
| Cushing's syndrome |
| Diabetes mellitus |
| Hypothyroidism |
| Kallman's syndrome |
| Primary amenorrhea |
| Pseudohypoparathyroidism |
| Turner's syndrome |
| Local diseases and mechanical obstruction of the airways |
| Adenoid hypertrophy |
| Allergic rhinitis |
| Atrophic rhinitis (Ozena) |
| Bronchial asthma |
| Deformity secondary to trauma |
| Exposure to toxic chemicals |
| Leprosy |
| Malignant disease of paranasal sinuses with extension into the nasal cavities |
| Nasal polyposis |
| Sinusitis |
| Sjogren's syndrome |
| Tumors of the nasopharynx with extension into the nasal cavities |
| Vasomotor rhinitis |
| Neurologic |
| Alzheimer's disease |
| Epilepsy |
| Head trauma |
| Huntington's chorea |
| Intracranial surgery |
| Multiple sclerosis |
| Parkinson's disease |
| Nutritional |
| Chronic renal failure |
| Cyanocobalamin (vitamin B12) deficiency |
| Korsakoff's psychosis |
| Pychiatric |
| Depression |
| Olfactory reference syndrome |
| Schizophrenia |
| Tumors |
| Intracranial: |
| Aneurysms of the anterior communicating bifurcation |
| Frontal lobe glioma |
| Hydrocephalus |
| Internal carotid aneurysms extending over the pituitary fossa |
| Neuroblastoma |
| Suprasellar meningioma |
| Sphenoidal ridge meningioma |
| Other meningiomas |
| Intranasal: |
| Adenocarcinoma |
| Inverted papilloma |
| Melanoma |
| Squamous cell carcinoma |
| Viral and infectious |
| Acute viral hepatitis |
| Herpes simplex |
| Influenza-like infections |
- Source: From Doty RL, Kimmelman CP. Smell and taste and their disorders. In: Asbury AK, McKhann GM, McDonald WI, eds. Diseases of the nervous system. Philadelphia: W.B. Saunders, 1986;469.
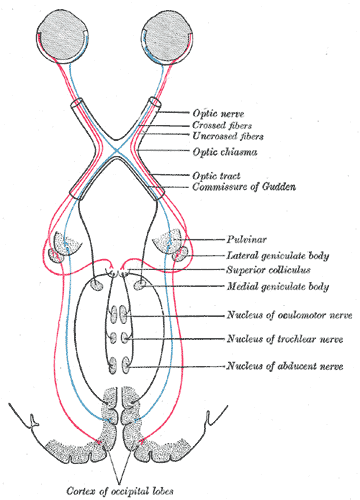

Transmits visual information from the retina to the brain. Derived from the embryonic retinal ganglion cell.
what is retinal ganglion cell.?
as we learn from histology...
It located in ganglion cell layer...whereby it consist few types of ganglion cell..lets c few types of it..(from wiki)
Based on their projections and functions, there are at least five main classes of retinal ganglion cells:
- Midget cell (Parvocellular, or P pathway; P cells)
- Parasol cell (Magnocellular, or M pathway; M cells)
- Bistratified cell (Koniocellular, or K pathway)
- Photosensitive ganglion cells
- Other ganglion cells projecting to the superior colliculus for eye movements (saccades)[2]

Damage to the optic nerve typically causes permanent and potentially severe loss of vision, as well as an abnormal pupillary reflex, which is diagnostically important. The type of visual field loss will depend on which portions of the optic nerve were damaged. In general:
- Damage proximal to the optic chiasm causes loss of vision in the visual field of the same side only.
- Damage in the chiasm causes loss of vision laterally in both visual fields (bitemporal hemianopsia). It may occur in large pituitary adenomata.
- Damage distal to the chiasm causes loss of vision in one eye but affecting both visual fields: The visual field affected is located on the opposite side of the lesion.
ROle in disease:
Injury to the optic nerve can be the result of congenital or inheritable problems like Leber's Hereditary Optic Neuropathy, glaucoma, trauma, toxicity, inflammation, ischemia, infection (very rarely), or compression from tumors or aneurysms. By far, the three most common injuries to the optic nerve are from glaucoma, optic neuritis (especially in those younger than 50 years of age), and anterior ischemic optic neuropathy (usually in those older than 50).
Glaucoma is a group of diseases involving loss of retinal ganglion cells causing optic neuropathy in a pattern of peripheral vision loss, initially sparing central vision.
Optic neuritis is inflammation of the optic nerve. It is associated with a number of diseases, the most notable one being multiple sclerosis.
Anterior Ischemic Optic Neuropathy is a particular type of infarct that affects patients with an anatomical predisposition and cardiovascular risk factors.
Optic nerve hypoplasia is the underdevelopment of the optic nerve causing little to no vision in the affected eye.
Optometrists and Ophthalmologists can detect and diagnose some optic nerve diseases but, those sub-specialists that are neuro-ophthalmologists, are often best suited to diagnose and treat diseases of the optic nerve.
Testing:
Visual acuity is tested in each eye separately. Ensure the patient's vision is corrected with eyeglasses or a pinhole. The patient is asked to read progressively smaller lines on the near card or Snellen chart.
Visual fields are assess by asking the patient to cover one eye while the examiner tests the opposite eye. The examiner wiggles the finger in each of the four quadrants and asks the patient to state when the finger is seen in the periphery. The examiner's visual fields should be normal, since it is used as the baseline.
Pupillary light reflex The patient stares into the distance as the examiner shines the penlight obliquely into each pupil. Pupillary constriction should be noted on the eye examined (direct response) and on the opposite eye (consensual response). The swinging flashlight test involves moving the light between the two pupils. Normally both direct and consensual responses are ellicited when the light shines on an eye, and some dilation will occur during the swing between.
III. Oculomotor Nerve
enter via superior orbital fissure and controls most of the eye's movements, including constriction of the pupil and maintaining an open eyelid
Nuclei
The oculomotor nerve (CN III) arises from the anterior aspect of mesencephalon (midbrain). There are two nuclei for the oculomotor nerve:
- The oculomotor nucleus originates at the level of the superior colliculus. The muscles it controls are the striated muscle in levator palpebrae superioris and all extraocular muscles except for the superior oblique muscle and the lateral rectus muscle.
- The Edinger-Westphal nucleus supplies parasympathetic fibres to the eye via the ciliary ganglion, and thus controls the sphincter pupillaemuscle (effecting pupil constriction) and the ciliary muscle (affecting accommodation).
Sympathetic postganglionic fibres also join the nerve from the plexus on the internal carotid artery in the wall of the cavernous sinus and are distributed through the nerve, e.g., to the smooth muscle of superior tarsal (Mueller's) muscle.
Ciliary Ganglion. Green = parasympathetic; Red = sympathetic; Blue = sensory
Emergence from brain
On emerging from the brain, the nerve is invested with a sheath of pia mater, and enclosed in a prolongation from the arachnoid.
It passes between the superior cerebellar (below) and posterior cerebral arteries (above), and then pierces the dura mater anterior and lateral to theposterior clinoid process, passing between the free and attached borders of the tentorium cerebelli.
It runs along the lateral wall of the cavernous sinus, above the other orbital nerves, receiving in its course one or two filaments from the cavernous plexus of the sympathetic, and a communicating branch from the ophthalmic division of the trigeminal.
[edit]Superior and inferior rami
It then divides into two branches, which enter the orbit through the superior orbital fissure, between the two heads of the lateral rectus.
Here the nerve is placed below the trochlear nerve and the frontal and lacrimal branches of the ophthalmic nerve, while the nasociliary nerve is placed between its two rami:
- superior branch of oculomotor nerve
- inferior branch of oculomotor nerve

Testing
[edit]Eye muscles
Cranial nerves III, IV, and VI are usually tested together. The examiner typically instructs the patient to hold his head still and follow only with the eyes a finger or penlight that circumscribes a large "H" in front of the patient. By observing the eye movement and eyelids, the examiner is able to obtain more information about the extraocular muscles, the levator palpebrae superioris muscle, and cranial nerves III, IV, and VI.Since the oculomotor nerve controls most of the eye muscles, it may be easier to detect damage to it. Damage to this nerve, termed oculomotor nerve palsy is also known by the down n' out symptoms, because of the position of the affected eye.[edit]Pupillary reflex
The oculomotor nerve also controls the constriction of the pupils and thickening of the lens of the eye. This can be tested in two main ways. By moving a finger toward a person's face to induceaccommodation, as well as his going cross-eyed, his pupils should constrict.Shining a light into one eye should result in equal constriction of the other eye. The neurons in the optic nerve decussate in the optic chiasm with some crossing to the contralateral optic nerve tract. This is the basis of the "swinging-flashlight test".
nnervates a single muscle: the superior oblique muscle..
Nucleus:
The nucleus of the trochlear nerve is located in the caudal mesencephalon beneath the cerebral aqueduct. It is immediately below the nucleus of theoculomotor nerve (III) in the rostral mesencephalon.
The trochlear nucleus is unique in that its axons run dorsally and cross the midline before emerging from the brainstem. Thus a lesion of the trochlear nucleus affects the contralateral eye. Lesions of all other cranial nuclei affect the ipsilateral side except the optic nerves - cranial nerve II - which innervate both eyes.
Clinical syndromes
[edit]Vertical diplopia
Injury to the trochlear nerve cause weakness of downward eye movement with consequent vertical diplopia (double vision). The affected eye drifts upward relative to the normal eye, due to the unopposed actions of the remaining extraocular muscles. The patient sees two visual fields (one from each eye), separated vertically. To compensate for this, patients learn to tilt the head forward (tuck the chin in) in order to bring the fields back together – to fuse the two images into a single visual field. This accounts for the “dejected” appearance of patients with “pathetic nerve” palsies.
As would be expected, the diplopia gets worse when the affected eye looks toward the nose – the contribution of the superior oblique muscle to downward gaze is greater in this position. Common activities requiring this type of convergent gaze are reading the newspaper and walking down stairs. Diplopia associated with these activities may be the initial symptom of a fourth nerve palsy.
Alfred Bielschowsky's head tilt test is a test for palsy of the superior oblique muscle caused by damage to cranial nerve IV (trochlear nerve).
[edit]Torsional diplopia
Trochlear nerve palsy also affects torsion (rotation of the eyeball in the plane of the face). Torsion is a normal response to tilting the head sideways. The eyes automatically rotate in an equal and opposite direction, so that the orientation of the environment remains unchanged – vertical things remain vertical.
Weakness of intorsion results in torsional diplopia, in which two different visual fields, tilted with respect to each other, are seen at the same time. To compensate for this, patients with trochlear nerve palsies tilt their heads to the opposite side, in order to fuse the two images into a single visual field.
The characteristic appearance of patients with fourth nerve palsies (head tilted to one side, chin tucked in) suggests the diagnosis, but other causes must be ruled out. For example, torticollis can produce a similar appearance.
VI. Abducens Nervecontrol lateral rectus mucle of the eye.
enter through superior orbital fissure.
 abducens nucleus is located in the pons, on the floor of thefourth ventricle, at the level of the facial colliculus
abducens nucleus is located in the pons, on the floor of thefourth ventricle, at the level of the facial colliculusV. Trigeminal Nerve
first of all,There is 3 branches for trigeminal nerve.
V1.Opthalmic
V2. maxillary
V3 Mandibular.
Function
The sensory function of the trigeminal nerve is to provide the tactile, proprioceptive, and nociceptive afference of the face and mouth. The motor function activates the muscles of mastication, the tensor tympani, tensor veli palatini,mylohyoid, and anterior belly of the digastric.

Lets see branches of V1.Opthalmic nerve

V2 Maxillary nerve
 3
3
V3 Mandibular nerve


VII. Facial Nerve

Most important 5 branches.. temporal,zygomatic,buccal,mandibular,cervical...

Branches:(from wiki)
Inside skull
- Greater petrosal nerve - provides parasympathetic innervation to several glands, including the nasal gland, palatine gland, lacrimal gland, and pharyngeal gland. It also provides parasympathetic innervation to the sphenoid sinus, frontal sinus, maxillary sinus, ethmoid sinus, nasal cavity, as well as special sensory taste fibers to the palate via the Vidian nerve.
- Nerve to stapedius - provides motor innervation for stapedius muscle in middle ear
- Chorda tympani
- Submandibular gland
- Sublingual gland
- Special sensory taste fibers for the anterior 2/3 of the tongue.
[edit]Outside skull
Distal to stylomastoid foramen, the following nerves branch off the facial nerve:
- Posterior auricular nerve - controls movements of some of the scalp muscles around the ear
- Branch to Posterior belly of Digastric muscle as well as the Stylohyoid muscle
- Five major facial branches (in parotid gland) - from top to bottom:
- Temporal
- Zygomatic
- Buccal
- Marginal mandibular
- Cervical branch
Branches of buccal nerve
| Muscle | Action |
|---|---|
| Risorius | Smirk |
| Buccinator | Aids chewing by holding cheeks flat |
| Levator Labii Superioris | Elevates upper lip |
| Levator labii superioris alaeque nasi muscle | Snarl |
| Levator Anguli Oris | Soft smile |
| Nasalis | Flare Nostrils |
| Orbicularis oris muscle | Purse Lips |
The marginal mandibular branch innervates the following muscles:[1]
- Depressor labii inferioris - lowers bottom lip down and laterally. Origin: Anterior part of oblique line of mandible. Insertion: Lower lip at midline, blends with muscle from opposite side.
- Depressor anguli oris (triangularis) - lowers the corner of the mouth down and laterally. Origin: Oblique line of mandible below canine, premolar, and first molar teeth. Insertion: Skin at the corner of mouth and blending with orbicularis oris.
- Mentalis - raises and protrudes lower lip as it wrinkles skin on chin. Origin: Mandible inferior to incisor teeth. Insertion: Skin of chin.
Testing
Temporal branches of the facial nerve, a patient is asked to frown and wrinkle his or her forehead.
Zygomatic branches of the facial nerve, a patient is asked to close their eyes tightly.
Puff up cheeks (buccinator)
i. Tap with finger over each cheek to detect ease of air expulsion on the affected side
• Smile and show teeth (orbicularis oris)
VIII. Vestibulocochlear Nerve
Symptoms of damage
Damage to the vestibulocochlear nerve may cause the following symptoms:
- hearing loss
- vertigo
- false sense of motion
- loss of equilibrium (in dark places)
- nystagmus
- motion sickness
- gaze-evoked tinnitus.[2]

 \
\
Branches
- Tympanic
- Stylopharyngeal
- Tonsillar
- Nerve to carotid sinus
- Branches to the posterior third of tongue
- Lingual branches
- A communicating branch to the Vagus nerve

The glossopharyngeal nerve is mostly sensory. The glossopharyngeal nerve also aids in tasting, swallowing and salivary secretions. Its superior and inferior (petrous) ganglia contain the cell bodies of pain fibers. It also projects into many different structures in the brainstem:
- Solitary nucleus: Taste from the posterior one-third of the tongue and information from carotid baroreceptors and carotid body chemoreceptors
- Spinal nucleus of the trigeminal nerve: Somatic sensory fibers from the middle ear
- Lateral Nucleus of Ala Cinerea: Visceral pain
- Nucleus ambiguus: The lower motor neurons for the stylopharyngeus muscle
- Inferior salivatory nucleus: Parasympathetic input to the parotid and mucous glands.

Effects of Damage and Clinical Test
The Glossopharyngeal nerve if damaged can have several effects on the human body. These effects include loss of bitter and sour taste, and impaired swallowing. The clinical tests to see if the Glossopharyngeal nerve has been damaged includes testing the gag reflex of the mouth. Ask the patient to swallow or cough, and Other signs include speech impediments. Finally, test the posterior one-third of the tongue with bitter and sour substances.
The vagus nerve includes axons which emerge from or converge onto four nuclei of the medulla:
- The Dorsal nucleus of vagus nerve - which sends parasympathetic output to the viscera, especially the intestines
- The Nucleus ambiguus - which gives rise to the branchial efferent motor fibers of the vagus nerve and preganglionic parasympathetic neurons that innervate the heart
- The Solitary nucleus - which receives afferent taste information and primary afferents from visceral organs
- The Spinal trigeminal nucleus - which receives information about deep/crude touch, pain, and temperature of the outer ear, the dura of the posterior cranial fossa and the mucosa of the larynx
Branches
- Auricular nerve
- Pharyngeal nerve
- Superior laryngeal nerve
- Superior cervical cardiac branches of vagus nerve
- Inferior cervical cardiac branch
- Recurrent laryngeal nerve
- Thoracic cardiac branches
- Branches to the pulmonary plexus
- Branches to the esophageal plexus
- Anterior vagal trunk
- Posterior vagal trunk
- Hering-Breuer reflex in alveoli
The vagus runs posterior to the common carotid artery and internal jugular vein inside the carotid sheath.
The vagus nerve supplies motor parasympathetic fibers to all the organs except the suprarenal (adrenal) glands, from the neckdown to the second segment of the transverse colon. The vagus also controls a few skeletal muscles, notable ones being:
- Cricothyroid muscle
- Levator veli palatini muscle
- Salpingopharyngeus muscle
- Palatoglossus muscle
- Palatopharyngeus muscle
- Superior, middle and inferior pharyngeal constrictors
- Muscles of the larynx (speech).
XI. Spinal Accessory
XII. Hypoglossal Nerve


I had my TL a little more than a year ago when my third child was born via c-section. I was not told ANYTHING about the possible side effects of having this procedure. Since then I have experienced heavy bleeding lasting sometimes 3 weeks out of the month, weight gain, severe mood swings. Severe cramping, changes to my libido, severe depression accompanied by suicidal thoughts, headaches, migraines, many new symptoms & older issues are now exacerbated. The father of two of my children doesn't want me anymore. I've become too much of a pain in the ass I guess. We don't talk. We don't sleep in the same bed. I think he might really think I am crazy... & maybe I am. I feel crazy a lot of the time.
ReplyDeleteI'm unpredictable. I feel so angry about the whole thing & now what was once a mild fear of doctors has exploded into full on white coat syndrome that causes me to have a panic attack/hypertensive emergency (severe increase in blood pressure) whenever I have to deal with them. I'm not sure what to do... I fear the next time I have to see a doctor I'll have a stroke or a heart attack from the stress & anxiety of it... what do I do? I take my time and keep searching on internet looking for natural healing that how I came across Dr Itua herbal center website and I was so excited when Dr Itua told me to calm down that he will help me with his natural remedy I put my hope on him so I purchase his herbal medicines which was shipped to my address I used it as prescribed guess what? I'm totally healed my cramp pain is gone completely I also used his Anti Bacteria herbal medicines it's works for me very well I want anyone with health problem to contact Dr Itua herbal center for any kind diseases remedies such as Parkinson, Herpes, ALS, MS, Diabetes, Hepatitis, Hiv/Aids,Cancers, Men & Women Infertility, I got his email address drituaherbalcenter@gmail.com he has any kind of herbal remedies for women & men also for our babes. I really miss my Hunni...he's a fantastic father & a good man. He doesn't deserve this. I feel like an empty shell of who I used to be...